Tongue ties and lip ties; are they causing sleep problems for your baby?
A mom emails me to say that she’s considering sleep training. Her baby is around four months old and she’s wondering if he’s hit the four month sleep regression. We book our consultation and the time comes for us to chat.
After we exchange pleasantries, I get down to business. I have already seen her intake form, and a detailed multi-day sleep log. I ask questions and find out that this baby was never a good sleeper.
This is pretty common with my clients. But in these situations, mom will tell me that when her baby was a newborn, baby was colicky and/or had reflux .
This is often the first red flag I see.
When I ask if baby was put on medication for the reflux, the usual answer is “yes, but I’m not sure if it worked.”
Second red flag.
I will then ask about breastfeeding and find out that there is a history of pain, bleeding, cracked nipples, over or under supply or supplementing with formula because she felt (or was told) that she wasn’t producing enough.
Third red flag.
As I go through my now standard questions that help me get to the bottom of where the sleep issues are stemming from, (I firmly believe every child can sleep well, but there is always *something* that is preventing it from happening) I will come across issue after issue that usually leads me to asking;
“Was your child ever evaluated for a tongue or lip tie?”
Silence.
And then either I hear;
“what’s that?” or,
“yes, but the ___ (insert doctor, doula, midwife, lactation consultant, nurse) said there wasn’t one.”
I will then spend some time explaining why I think their child may have some sort of oral restriction.
They are often in disbelief or frustrated that something so simple may have been missed by the multiple health professionals they’ve seen.
And although they came to me believing there was a sleep issue, in situations where oral restrictions are present, it’s a feeding issue that is the root cause.
We will further examine the relationship between feeding, sleeping and ties in a bit. But first, let’s look at the basics of tongue, lip and buccal ties.
The Name Game
The first thing we need to know are some of the terms commonly used.
Frenum: This is the general term given to any fold, band of tissue or mucus membrane, in the body that attaches or anchors to a semi-mobile organ in the body.
Frenulum: A small frenum. The terms “frenum” and “frenulum” are often interchanged.
Lip Ties: This is when the lip (labial) frenulum is restricted or tight. Referred to as; upper labial tie (ULT), maxillary (upper) or mandibular (lower) or a combination of the terms.
Tongue Ties: Also known as ankyloglossia, or lingual ties.
Cheek Ties: These are often called buccal ties.
Tethered Oral Tissues (TOTs): A term referring to any ties located in the mouth.
Tongue, Lip and Buccal Ties-What Are They?
An oral tie, is a condition that refers to restricted movement of either the lip, tongue or cheeks due to a short, thick or tight frenulum. While we all have frenulums, they are only considered “tied” when movement or function is prevented or impaired.
Tongue Ties
Medically known as Ankyloglossia, a tongue tie is identified when the tongue’s movement and function is restricted due to a tight, short or thick lingual frenulum. A list of symptoms also needs to be present in order to make the diagnosis.
When the lingual frenulum is normal, it doesn’t hinder the full movements of the tongue; side to side, up, down and out. This means that there are no issues with children sucking, eating, swallowing and speaking.
But when there are tongue ties present, they can negatively effect a baby’s ability to latch, suck, feed and swallow. (Older children may also have difficulties with eating, chewing, nasal breathing, speech and dental alignment).
Classification of Tongue Ties
While the term “tongue and lip tie” is beginning to become more common, there are still many components that are misunderstood. One such example is identification.
Dr. Larry Kotlow, a pediatric dentist and one of the leading experts in TOTs, has devised a classification system based on the location of where a tie attaches, that many (but not all) TOTs experts use. However, this is not a classification of severity, but location only.
Classes 1 and 2 are anterior tongue ties. Classes 3 and 4 are posterior tongue ties. And in case you were wondering what’s the difference is, read on…
Anterior tongue ties – This type of tongue tie is very much visible and most commonly detected.
- It is either at the tip of the tongue (Class 1) (sometimes resulting in a heart-shaped tongue tip) or, just behind the tip of the tongue (Class 2).
- Class 1 ties are usually the only ones that some medical professionals consider a “real” tie, leading to many parents’ concerns being dismissed. However, some leading experts feel that every anterior tie also has a posterior component to it as well.
Posterior tongue ties – This type of restriction is under the tongue and not as easily identified.
- Here the membrane is less visible (Class 3), or hidden completely (Class 4).
- It is under the tongue and in the case with Class 4s, needs to be gently pushed down at the base and sides to be seen.
- Unless a health professional has specific training in tie identification, posterior tongue ties are most often missed.
How about Lip Ties?
We get a diagnosis of a lip tie when the labial frenulum attaches under the top lip to somewhere on the gums near the front teeth, causing restriction and tightness, along with an array of symptoms to both mother and child.
While many children have prominent labial frenulums, not all are considered restricted. This is why it takes an expert to assess how tight the restriction is, location of attachment in combination of symptoms noted by parents.
Similar to tongue ties – some professionals use a lip tie classification system. Again, this does not define the severity of the lip tie, but rather where the frenulum attaches to the lip.
- Class 1 – This type of lip tie is very rare and has little to no visible attachment.
- Class 2 – The attachment occurs somewhere on the gum line but above the edge of the gum line.
- Class 3 – The tie attaches to the edge of the gum line in line with a structure called the anterior papilla
- Class 4 – This type of tongue tie wraps right around to the hard palate.
Many parents will be confused as to whether or not their child has an actual lip tie, and not just a normal upper labial frenulum. For further readying, this is a wonderful article from Dr. Bobby Ghaheri, an ENT and another leading expert on ties, that talks in depth about the difference; The Difference Between a Lip Tie and a Normal Labial Frenulum.
Buccal Ties
Buccal or cheek ties are the least known of all the restrictions. This is when a small piece of tissue is attached from the inner cheeks to the gums.
They can be located anywhere from way in the back beside where the molars will eventually erupt, to closer to the front of the mouth. To identify these, a practitioner may have to gently hook their finger into the side of the mouth and lift up and outwards.
They don’t seem to cause as much trouble, however, they are the least known of all TOTs, and therefore, the least studied.
The Mighty Tongue
How many of us think about our tongue?
Not many, I would guess.
It may seem rather unimportant, but it is anything but. The tongue is comprised of eight muscles that connect to various parts including the hyoid bone and the skull, but it is the only muscle that isn’t connected to bone at both ends. (Want to know more about the muscles in the tongue, check out this video!)
Although we think of our tongue as primarily used for tasting food, it is also important for speech, sound formation and aids in chewing.
Lesser known, but also extremely important is that the tongue helps to shape our airway by always resting against the palate (roof of the mouth) keeping it wide and flat.
Proper resting oral posture should always be; lips closed and tongue fully against the roof of the mouth. But when a tongue is restricted, it may prevent this from happening leading to a high and narrow palate and potentially constricting the airway.
Tongue Tie and Lip Tie Symptoms
Since breastfeeding (and bottle feeding as well) requires the middle of the tongue to lift up to form a seal and suction, many tied babies are not able to feed efficiently due to the restriction of the tongue. This can be happening even if the child is gaining weight.
(This can be for several reasons. In the newborn stage, often mom’s supply is being maintained by hormones, so the baby doesn’t have to work very hard to receive milk, but issues can develop closer to four months of age when supply begins to be regulated by baby.
Older babies may start to increase the amount of feeds during the day and night in an effort to meet their needs.)
To a similar extent, the lips also play an important role in proper feeding. When one of these two components aren’t functioning properly, we can see a whole host of problems begin to emerge.
Here is a list of common symptoms tied babies may experience.
Tongue Ties and Sleep; What’s the Connection?
Many of the children that come to me who aren’t sleeping well, particularly around the fourth month, exhibit symptoms of having oral restrictions. It has become a chicken-and-egg scenario that looks like this;
- Baby can’t nurse or drink properly due to poor seal/suction on bottle or breast.
- Baby falls asleep feeding, but only sleeps enough to take the “edge” off, not to fully satisfy their sleep needs
- Baby wakes crying and mom feeds but baby can’t control flow from breast or bottle and pulls off, cough, chokes or gags
- Baby tries to compensate by using lips, cheeks or gums to extract milk
- Mom is experiencing painful nursing sessions, but has been told this is normal.
- Baby tires easily from working hard to drain breast or bottle, falls asleep before feed is complete
- Since they aren’t taking in the proper amount of calories at each feed, very short naps (usually under 30 minutes) and multiple night wakings result.
- Baby also may inhale a lot of air when feeding, leading to discomfort
- This causes excess air being ingested that results in reflux-like symptoms, the need to burp frequently and/or a gas that hinders the child from sleeping well due to discomfort.
- Baby is continually tired from the lack of restorative sleep
- To counter the building sleep deprivation, the brain increases the amount of cortisol and adrenaline that is released, further leading to shallow and unrestorative sleep
- A combination of severe sleep deprivation, insufficient calorie intake, discomfort from excess gas, lead to the inability to sleep deeply or fully.
- This causes short naps, multiple night wakings (more than what is considered “average” for the age) and early morning starts.
- Parents are dismissed and may be told this is all normal and “just how babies are”, leading to extreme sleep deprivation on the part of the parent.
- Parents may fall victim to risky behaviours, in an effort to cope with a wakeful baby and their exhaustion.
How Sleep Problems Escalate
As parents become desperate to help their babies sleep, they begin to try all sorts of props, gadgets and methods. Unfortunately, this then develops the child’s dependency on sleep associations.
Overtime, these sleep associations become habits that are deeply entrenched in the child’s sleep routine and it becomes a murky issue for parents to try and make sense of.
Further challenges erupt when the pediatrician has given the all-clear to night wean, either because the child’s weight gain is high or the baby has reached the six to eight month mark. Parents try, and it results in a very stressful night for all involve.
Can a Tied Baby Be Sleep Trained?
I help children sleep better by having a holistic approach rooted in sleep hygiene and sleep science. This means that my focus is always on when and how naps and bedtime are starting and lasting.
Timing and quality of sleep is a crucial component for a strong sleep foundation.
The actual sleep training method (ie Timed Intervals, Chair Method, Extinction, Pick Up, Put Down, No/less-Cry), is the LAST consideration.
If a parent chooses to sleep train, it is only appropriate for four months and older, and only to wean sleep associations.
Sleep training does not fix wakings due to sleep deprivation or hunger.
My focus is always primary based on making sure our little ones are not sleep deprived. So if you’re asking if a tied baby regardless of age, can learn to sleep better; absolutely yes.
But if you’re asking if a tied baby can learn to sleep completely through the night, without any feeds, then I will say “usually not”. And almost definitely not if they are under six months of age.
Of course each child is different and the severity of restriction needs to be taken into account. But as a general rule, I usually ask families of suspected tied babies to add more night feeds, not less.
If a baby is waking out of hunger, then trying to wean those feeds is unfair and unrealistic. (However, I am not a consultant that pushes night weaning even in untied babies. I know that sleep training and night feeds are not mutually exclusive.)
So if you suspect your baby may have an oral restriction; fear not. We can we get them on a more healthy sleep routine, reduce (but likely not eliminate) the amount of times they are waking at night, and help them to nap longer.
How To Help a Tied Baby Sleep Better
Ok, so the next question is, how?
We do this by following the basics of healthy sleep hygiene. That is, create good sleep habits.
Good day, sunshine: Start with having regular morning wake up times, which after four months of age, tends to average somewhere between 6-7:30am.
Sleep Ritual: Create a soothing wind down routine that is relaxing and comforting. This helps the child to associate the routine with sleep.
Location, location, location: Have your child nap in a location that is comfortably cool and very dark. Doing so kick starts the natural melatonin production and encourages the wonderful deep sleep that the body and brain craves.
Encourage restorative naps: This means that on average, your baby’s naps are lasting longer than an hour. If your child is on three nap-a-day routine, the first two tend to be the long naps, and the third nap is shorter; about one sleep cycle.
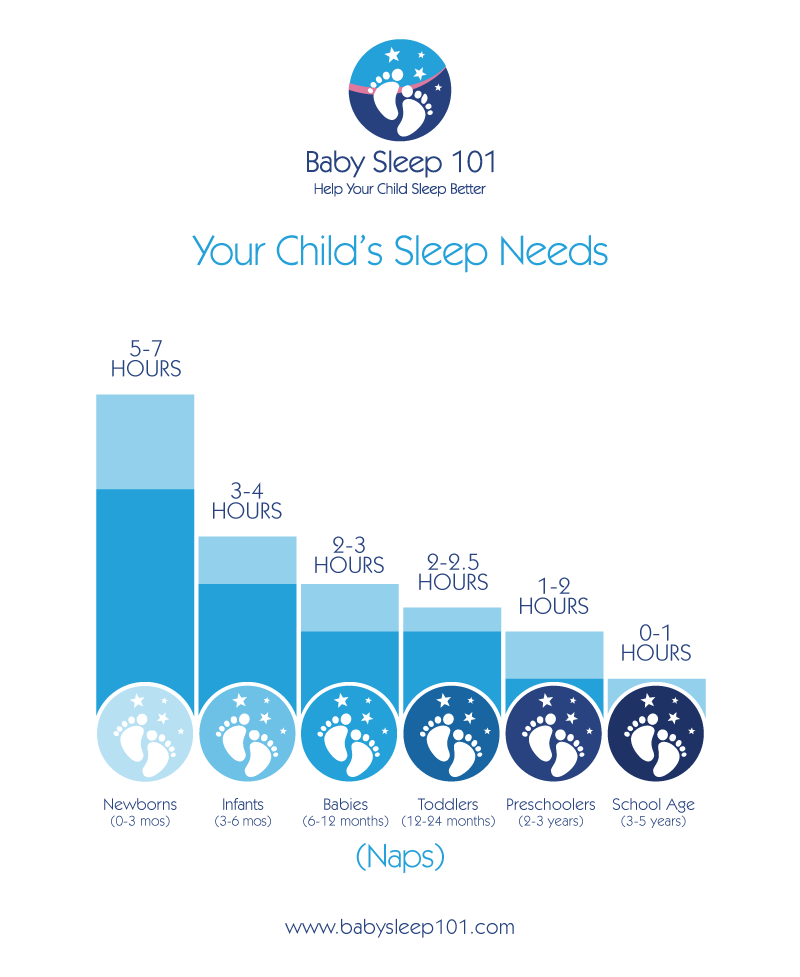
Don’t worry about trying to lengthen this third nap-just let it be short. Want to know how many of hours of daytime sleep your child should be averaging? See below…
Timing is important: We also want to have naps that are well-timed with the child’s sleep circadian rhythms (if older than four months old) so that the sleep that they do take is as refreshing as possible.
Keep wake periods age-appropriate: If we keep babies up too long in between naps on a regular basis, it will further add to their sleep debt levels. This will cause extra crying and resistance during the wind down.
Early bedtime: Finally, to help manage the sleep debt, we must make sure to adjust bedtime to the quality and quantity of daytime sleep. That means, if naps have been short and unrestorative, bedtime must be earlier than usual to accommodate for the missing sleep. Sometimes this may only be twenty minutes and sometimes it’s two hours. It really depends on the child’s age and nap quality.
What To Do If You Suspect Your Baby Has a Tongue or Lip Tie
If you are nursing, an International Board Certified Lactation Consultant (IBCLC), who has taken additional studies in tethered oral ties, should be seen to assess latch, position, form and structure as they can often offer mothers ways to help baby feed more efficiently (even with bottles!).
In some parts of Canada and the US, Speech-Language Pathologists or Oral-Myofunctional Therapists may also be certified to do oral assessments. Alternatively, there are a number of pediatric dentists becoming tie savvy and performing exams.
Regardless of the practitioner, a comprehensive exam of the baby’s mouth including upper and lower lips, cheeks, tongue mobility, lift and reach should be checked.
Sometimes I hear of practitioners only checking if a baby can stick their tongue out. However, proper oral resting posture, nursing and later, speech, all require the mid part of the tongue to freely lift up, not out.
Feeding should be assessed, as should body structure to evaluate for any tension or tightness. Finally, all of mom and baby’s symptoms should also be documented.
After the evaluation, the IBCLC, SLP or OMT will refer you to a release provider. In addition, usually some sort of bodywork is prescribed to help baby with any tension they may be experiencing from trying to compensate with the restriction. This may be cranial sacral therapy, osteopathy, or pediatric chiropractic care.
I have seen many posts in social media groups asking for other members (who are not certified practitioners) to identify tongue ties based on a picture. However, to have an accurate diagnosis, an examiner should do a full investigation on function, not just form. Just because you see a frenulum in your child’s mouth, does not mean they have a tie.
While social media can help point us in the right direction, a well-trained professional must still fully assess your baby’s mouth, including upper and lower lips, under the tongue and cheeks.
Many practitioners will also use one of more assessment tools/forms/checklists that have been established to help diagnose a restriction. Some common ones are;
Carole Dobrich’s: Frenotomy Decision Tool for Breastfeeding Dyads
Carmen Fernando’s Tongue Tie Assement Protocol (TAPs),
Alison Hazelbaker; Hazelbaker Assement Tool For Lingual Frenulum Function (HATLFF)
Lingual Frenulum Protocol by Martinelli and Marchesan
Where Can I Find More Information?
Knowledge is power. The more you know, the better.
Here are some further resources for you….
Dr. Bobby Ghaheri: Website, Facebook Page
Dr. Larry Kotlow: Website, Facebook Page
Dr. Soroush Zaghi: Website
Tongue-Tied: How a Tiny String Under the Tongue Impacts Nursing, Speech, Feeding and More
Tongue Tie: From Confusion to Clarity
Tongue Tie Babies Facebook group has links to local chapters and providers. American based, but has links to other countries.
Canadian Tongue Tie Facebook group also has resources and information on providers, categorized by province.
Research:
- The Evidence Supports Treating Tongue Tie For Breastfeeding Problem
- The Effects of Office-Based Frenotomy for Anterior and Posterior Ankyloglossia on Breastfeeding
- Management of Posterior Ankyloglossia using the Er,Cr:YSGG Laser
- Efficacy of Neonatal Release of Ankyloglossia: A Randomized Trial
- Tongue Tie and Frenotomy in the Breastfeeding Newborn
- Ankyloglossia, Exclusive Breastfeeding and Failure to Thrive
- The Influence of the Maxillary Frenum on the Development and Pattern of Dental Caries on Anterior Teeth in Breastfeeding Infants: Prevention, Diagnosis and Treatment Posterior Ankyloglossia: A Case Report
- Nipple pain at presentation predicts success of tongue-tie division for breastfeeding problems
- Frenulotomy for Breastfeeding Infants with Ankyloglossia: Effect on Milk Removal and Sucking Mechanism as Imaged by Ultrasound
- Tackling Ankyloglossia in the Office
- Ankyloglossia in Breastfeeding Infants: The Effect of Frenotomy on Maternal Nipple Pain and Latch
- Immediate nipple pain relief after frenotomy in breast-fed infants with ankyloglossia: A randomized, prospective study
- Tongue-tie division in infants with breastfeeding difficulties
- Randomized, controlled trial of division of tongue-tie in infants with feeding problems
- Tongue Tie
- Ankyloglossia: the adolescent and adult perspective
- The effect of ankyloglossia on speech in children
- Ankyloglossia: assessment, incidence and effect of frenuloplasty on the breastfeeding dyad
- Breastfeeding Difficulties as a Result of Tight Lingual and Labial Frena: A Case Report
You and Your Family Can Sleep Again!
The world of tethered oral tissues can seem overwhelming at first. I know, I’ve been there first hand with my own children, and with countless other parents who have sought out my help.
It can be confusing to try and sort things out. You may have just come to terms with thinking your child has some challenges with sleep, but now may realize that it may be rooted in a different issue altogether.
However, the good news is, you are not alone! Whether tongue, lip or buccal ties, there are more people becoming aware of their impact.
There are many parents going through what you are. And while, it can be tricky to find them, thanks to the wonders of the internet, there are many professionals that can help you on this journey.
If you suspect a TOTs issue, seek out a practitioner near you and have your little one examined. That way, you and your family can get the sleep you all deserve and need.
Need more help with getting your child’s sleep on track, even if they have tongue ties or other oral restrictions? You don’t have to suffer with sleep deprivation. Here are some free resources for you…
Newborn sleep? Download your free newborn guide here.
Baby sleep? Download your free baby guide here.
Toddler and Preschooler sleep? Download your free toddler and preschooler guide here.